|
Eran S. Zacks, MD, Daniel P.
Morin, MD, Shaun Ageno, MD, Matthew Janik, MD, Daniel J. Cantillon, MD,
Andreas C. Mauer, MD, Steven M. Markowitz, MD, Suneet Mittal, MD, Sei Iwai,
MD, Bindi K. Shah, MD, Kenneth M. Stein, MD and Bruce B. Lerman, MD. Cornell
University Medical Center, New York, NY
|
|
Background: T-wave
alternans testing (TWA) has been proposed as a non-invasive method for risk
stratification in pts with depressed LVEF. Prior investigation has shown
that IV beta-blockers (BB) decrease the positivity rate of TWA in pts at
electrophysiology study (EPS). The purpose of this study is to evaluate the
influence of chronic oral BB on TWA.
Methods: We prospectively evaluated 251 pts with CAD, LVEF <40%,
and NSVT (203 men, age 66.6 +/-10.5 yrs) who underwent EPS and were
followed for > 2 yrs. TWA was performed using an atrial pacing
protocol (CL:550 ms) and interpreted using standard criteria. The BB+ group
was on oral BB at the time of EPS and the BB- group was off BB for >24
hrs. TWA positive and indeterminate results were grouped as non-negative
based on prior convention. Follow-up for VT, VF, and death was obtained
from chart review, device interrogation and social security death index.
Sensitivity and specificity for TWA were calculated in the BB+ and BB-
groups based on event-free 2-yr survival.
Results: The BB+ group had 210 (84%) pts and the BB- group had 41
(16%) pts. There were no significant differences between the two groups
with regard to age, gender, LVEF, or ICD implant rate. The indeterminate
rates for BB+ and BB- groups were comparable (28% vs. 27%, p=1.00). The BB+
and BB- groups had 144 (69%) pts and 28 (68%) pts with non-negative results
respectively (p=1.00). There were 36 (17%) events in BB+ pts and 6 (15%)
events in BB- pts (p=0.448). The sensitivities and specificities of TWA for
2-yr VT/VF-free survival did not differ significantly between the BB+ and
BB- groups (sensitivity: 75% vs. 83%, p=0.557, specificity: 33% vs. 34%,
p=0.503).
Conclusions: Chronic oral BB at the time of testing does not
significantly influence the non-negative rate, sensitivity, and specificity
of TWA. These findings suggest that there is no need to discontinue oral BB
prior to TWA using an atrial pacing protocol. 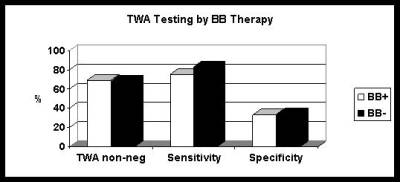
|
|
|